How Long to Continue Progesterone Suppositories
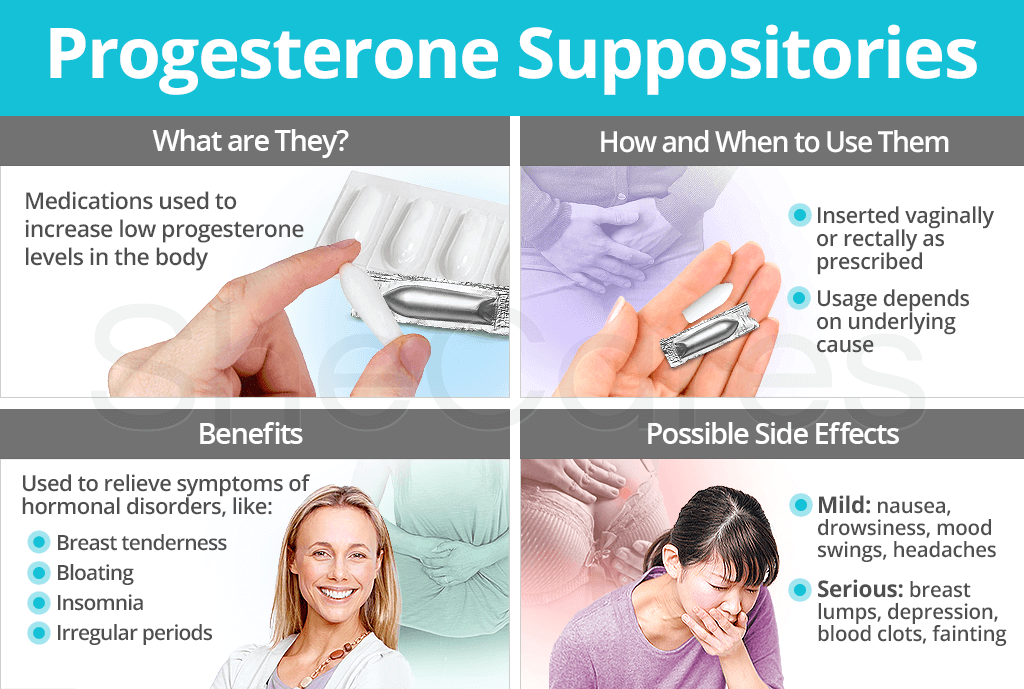
Although often overlooked, progesterone suppositories are a viable option for treating a progesterone deficiency invoked by a variety of hormonal disorders. Continue reading to discover more about progesterone suppositories, such as what they do, how and when they are used, and where to purchase them.
Progesterone suppositories are solid unit dosages intended for application into body orifices, namely the vagina or rectum. Once inserted, they release progesterone over a prolonged period of time, allowing the hormone to be absorbed at a slow and steady rate.
Vaginal progesterone suppositories. Vaginal suppositories are can be inserted with an applicator or the index finger, depending on the size. They are designed to dissolve in mucous membrane secretions.
Rectal progesterone suppositories. Rectal suppositories are inserted up to an inch within the sphincter. They are cone-shaped and designed to melt at body temperature.
What do Progesterone Suppositories Do?
Progesterone suppositories are used to treat many hormonal irregularities, such as luteal phase defect, luteal phase spotting, and PMS, among others.
How Do I Take a Progesterone Suppository?
As aforementioned, progesterone suppositories may be inserted vaginally or rectally. Use them at evenly spaced intervals or as prescribed the same time each day.
For vaginal suppositories, an applicator assists with insertion of the medication into the vagina, similar to a tampon. This is usually performed two to three times daily. 1 To avoid drainage after insertion, insert the suppository lying down. For this reason, it is often put in right before bedtime or when resting.
For rectal suppositories, the insertion process is much the same as vaginal suppositories. However, it is normally performed with the index finger instead of an applicator. Buttocks should be clenched together for a few seconds after insertion to assure the suppository does not come out.
When Do I Use a Progesterone Suppository?
For hormonal disorder treatment, progesterone suppositories are generally prescribed for only 6 to 12 days at a time. When used as part of a fertility treatment, women may continue use for up to 12 weeks into the pregnancy.
Some mild side effects of suppositories include nausea, breast tenderness, drowsiness, mood swings, vaginal discomfort, irritability, or headaches, among others.
For specific use, this progesterone treatment may be used during early pregnancy, but under the supervision of a doctor. Women who are breastfeeding should be wary as the progesterone from suppositories does pass into breast milk.
More severe side effects include yellowing eyes and skin, breast lumps, depression, swelling of the ankles or feet, blood clots, coughing up blood, fainting, trouble breathing, slurred speech, and more.
Progesterone suppositories can be obtained with a doctor's prescription or over the counter at pharmacies and major online retailers. Use of over-the-counter progesterone suppositories should be consulted with a doctor for proper dosing. Improper usage can evoke various side effects.
In sum, similar to other progesterone treatments, progesterone suppositories - either administered vaginally or rectally - are used to treat symptoms brought on by hormonal disorders. Depending on the reason for usage, progesterone suppositories can be used for as little as two weeks to as long as three consecutive months. Women should be monitored throughout the treatment period for varying side effects that may evolve. This form of progesterone medication is available through prescription or over the counter.
Find out how to naturally increase progesterone levels and evade unwanted side effects with progesterone supplements, which include a selection of herbal options.
- Hanan, Z.I. & Durgin, J.M. (2015). Pharmacy Practice for Technicians, Fifth Edition. New York: Cengage Learning. Available from Google Books.
- Michigan Medicine. (2015). Progesterone vaginal. Retrieved December 6, 2019, from http://www.uofmhealth.org/health-library/d00550t1
- Moini, A. et al. (2011). Comparing intramuscular progesterone, vaginal progesterone and 17 -hydroxyprogestrone caproate in IVF and ICSI cycle. Iranian Journal of Reproductive Medicine, 9(2), 119-124. Retrieved December 6, 2019, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4216446/
- The National Infertility Association. (n.d.). Luteal Phase Defect. Retrieved December 6, 2019, from https://resolve.org/infertility-101/medical-conditions/luteal-phase-defect/
- Office on Women's Health. (2017). Premenstrual syndrome (PMS). Retrieved December 6, 2019, from https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome
- White, L. et al. (2011). Foundations of Basic Nursing, Third Edition. New York: Cengage Learning. Available from Google Books.
- Yassaee, F. et al. (2014). The Effect of Progesterone Suppositories on Threatened Abortion: A Randomized Clinical Trial. Journal of Reproduction & Infertility, 15(3), 147-151. Retrieved December 6, 2019, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4138421/
Footnotes:
- Government of Alberta. (2016). Progesterone Suppository - Vaginal. Retrieved December 6, 2019, from https://myhealth.alberta.ca/health/medications/pages/conditions.aspx?hwid=fdb0975&
juarezcoatseardeas.blogspot.com
Source: https://www.shecares.com/hormones/progesterone/suppositories
0 Response to "How Long to Continue Progesterone Suppositories"
Postar um comentário